Several months ago a patient in her first trimester of pregnancy asked me about a new product called E3Live® BrainON®, and was wondering if this product was safe her to take. Many of her friends were taking it, and she was wondering about a convincing testimonial from an Evita Ramparte on the E3Live® website.
I went through my entire pregnancy drinking E3Live® Enhanced with BrainON, which kept my mind alert, awake and positive. I gave birth to [a] very healthy baby boy. I am breastfeeding, and I believe it is thanks to E3Live® that I have plenty of milk and no post-partum depression. We’re in good spirits and good health. Besides, I have already lost all the weight I gained in pregnancy! As a wellness journalist, I am often asked whether E3 is safe for pregnant and nursing moms. On the bottle, it’s written: ‘Consult your physician.’ Unfortunately, few physicians know about this beautiful gift of Nature. Naturally, they are afraid to recommend something they have not studied.
That’s quite an endorsement, which might allay the concern of any pregnant mom, but it’s also pre-emptive shot-across-the bow against any rational critique of this product. It’s like Ms. Ramparte is telling us that E3Live® BrainON® is something so unique and so different, that science truly cannot understand it’s virtue and benefits, that it lies beyond any kind of logical explanation. But taking a look at the ingredients, I don’t see anything heretofore unknown to science. In fact, I see something rather concerning – especially for my pregnant patient.
According to the website, E3Live® BrainON® is stated on the website to contain “Organic, liquid fresh-frozen AFA algae (Aphanizomenon flos aquae) with BrainON®, an organic AFA extract of Phenylethylamine (PEA).” Let’s examine these two ingredients in detail:
Aphanizomenon flos aquae
The first ingredient, Aphanizomenon flos aquae (AFA), is a blue-green algae or cyanobacteria, that used to be sold under the trade name “Super Blue-Green Algae®” in the early 1990s when I was training as a herbalist. I recall that it was popular among some of the students, and lots of people were talking about it: not surprising given that it was sold as part of an MLM scheme. But I felt wary of this product, just like I did with grapefruit seed extract, which was also becoming popular at the time. Among its most vociferous adherents in my class was a young woman who claimed to have stacks of research papers on SBGA® – unfortunately, she only lasted a few months before having to bow out due to sickness. It was a short time later that we learned of major problems with AFA, as detailed by John M. McPartland (DO) in the Townsend Letter for Doctors:
“A. flos-aquae also produces hepatotoxins and neurotoxins. Some of these are carcinogenic.(6b) Others are acutely lethal. The LD50 of one hepatotoxin, microcystin-LR is a mere 50 µg/kg, compared to cyanide’s LD50 of 10,000 µg/kg.(7) Neurotoxins produced by A. flos-aquae include neosaxitoxin and anatoxin.(8) Anatoxin is a chemical cousin to cocaine. Anatoxins may be the reason why people eating blue-green algae sometimes feel energized. Some people also describe being addicted to blue-green algae. Animals are known to develop a fatal attraction to mats of blue-green algae washed up on shorelines.(9) Anatoxins are neurotoxins and eventually destroy brain cells.(10) And contrary to claims by Cell Tech, toxins have been found in A. flos-aquae coming from Klamath Lake.(6,11,12) Cell Tech reportedly tests their algae for these toxins. But in 1984 batches of blue green algae distributed by Cell Tech were found to be toxic and seized by the FDA.”
While Super Blue-Green Algae® is no longer available, it has been reinvented in products such as E3Live® BrainON®, which uses the same species of cyanobacteria that Dr. McPartland refers to in his article. And while the company that makes it, Klamath Algae Products Inc., claims that it is safe, and has many testimonials to back it up, they don’t publish the actual level of these hepatotoxins and neurotoxins in their product. I contacted the company in April of 2013, and asked them for these details, because I was concerned for my pregnant patient. When I first called, the customer service representative hadn’t any clue what I was asking for, but reassured me that E3Live® BrainON® was a great product. Later, I received an email from an E3Live® rep, who forwarded me first a simple monograph, but when pressed for actual data, sent me a “certificate of analysis”:
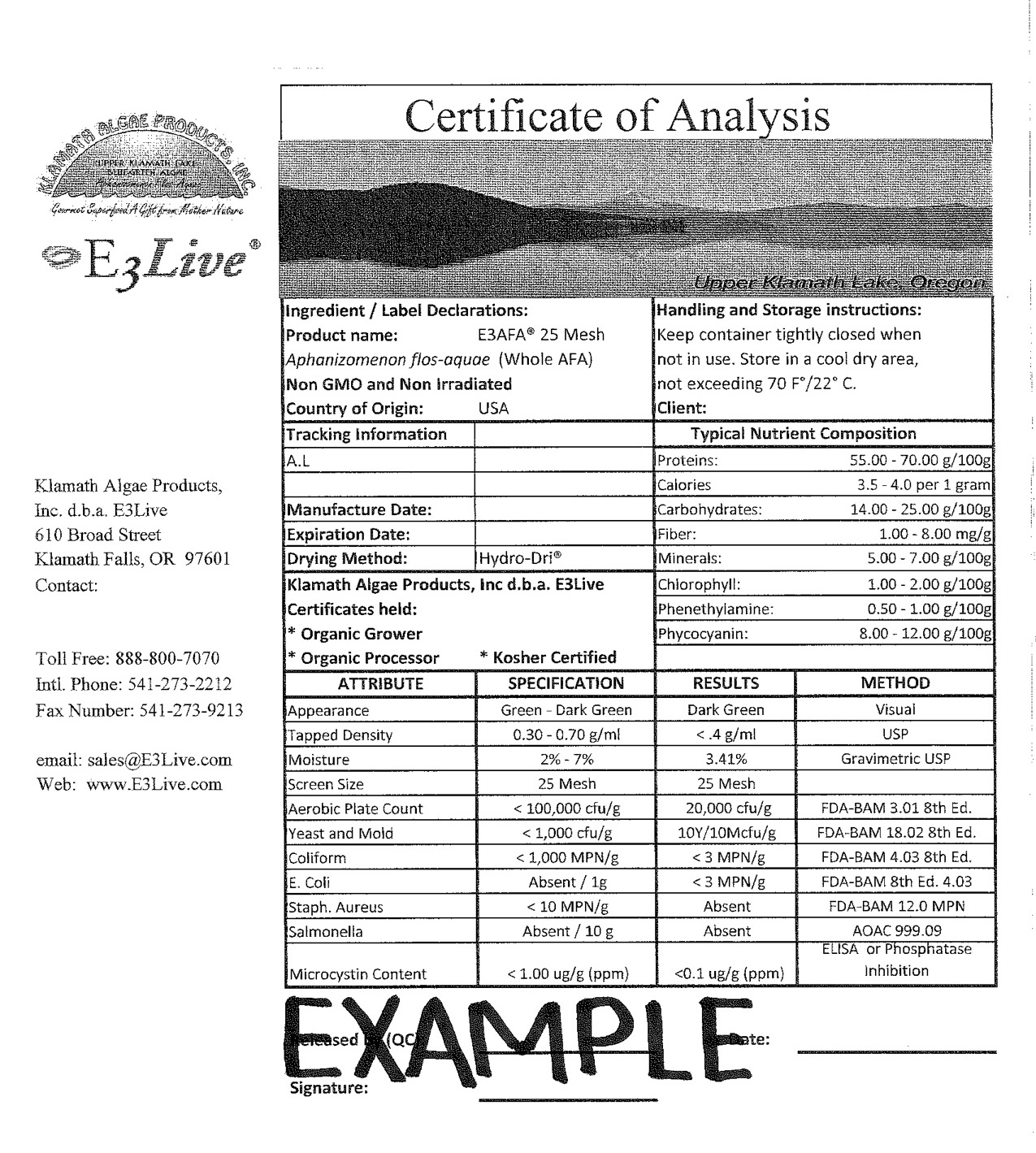
This “certificate of analysis” isn’t helpful of course, because it is just an example. Again, I wrote E3Live® again for the actual data, but as of yet I have not heard back from the E3Live® rep. As you can see in the analysis they provided, E3Live® states that they test for microcystin, a toxic peptide that is highly toxic to the liver. The regulatory limit for microcystin established by the Oregon Health Division and the Oregon Department of Agriculture is 0.1 micrograms per gram. Microcystin levels above this limit thus represent a risk to the consumer, and the higher the levels, the greater the risk.
Most retail products containing Aphanizomenon flos aquae are sourced from Klamath Lake, in Oregon. Locals to the area are well aware of frequent public health notices, warning recreational users about the danger of algal blooms in Oregon, which is well established to cause a variety of health issues including diarrhea, cramping, vomiting, fainting, numbness, dizziness, tingling and paralysis. Under the current regulations, however, AFA has received an exemption from the Oregon Health Authority:
Aphanizomenon flos-aquae (AFA) is a species of cyanobacteria commonly found in Oregon’s fresh waters. Although some studies have shown this species to produce toxins in other parts of the world, subsequent evaluations of that work show that the species either was or likely was misidentified. For the purpose of issuing public health advisories, AFA is excluded from calculation of combined cell counts of toxigenic species.
While this seems to provide some reassurance, and perhaps reflects the influence of a powerful stakeholder, other research continues to identify problems with products containing AFA. In 2008, the Universität Konstanz in southern Germany found microcystin levels that exceeded the safety level of 1 microgram microcystin per gram in 10 out of 16 samples of AFA sourced from Klamath Lake. In a more recent study in Italy, an analysis of 17 different brands of AFA-containing products were found to be “contaminated by highly variable levels of microcystins (MC-LR and MC-LA congeners), up to 5.2 μg MC-LR equivalents per gram product”. In the WHO’s Guidelines For Drinking-water Quality (3rd ed.) (p. 280), naturally-occuring toxins in Aphanizomenon species include not just peptides like microcystins, but alkaloids such as anatoxin-A, the saxitoxins, and cylindrospermopsin, none of which are listed in the “certificate of analysis” from E3Live®. But it starts to get even worse. Although E3Live® BrainON® is supposedly safe for pregnancy, another study has showed that AFA contains high levels of retinoic acid, a well-established reproductive toxin (teratogen) that promotes birth defects of the nervous system, skeleton, heart, thymus, and urogenital system, in all types of vertebrates, including humans. And even after you remove all these toxins, in study of 259 people using a detoxified extract of Aphanizomenon flos aquae, AFA still caused an allergic reaction in 12% of the population. If you are offering advice to a pregnant woman, does any of this sound safe to you?
Phenylethylamine
The product information for E3Live® BrainON® also states that it contains phenylethylamine (PEA), a monoamine alkaloid that naturally occurs in the brain, acting both as a neuromodulator and neurotransmitter. Similar to amphetamine in action, PEA is synthesized in the brain from the amino acid phenylalanine, and stimulates the release of norepinephrine and dopamine, just like cocaine and methamphetamine. In this way, PEA is a “feel-good” substance when secreted in the brain. In their marketing, the manufacturer claims that E3Live® BrainON® contains a natural-sourced PEA, and on the surface, I didn’t find this too surprising. PEA is found in a variety of plants such as cacao bean, and at one time, was a proposed as a mechanism for the mood-enhancing effects of chocolate. While I searched extensively for published research on the natural occurrence of PEA in Aphanizomenon flos-aquae, the only reference I could find was a patent filed in 2009, and a questionable wikipedia citation. The patent refers to a propriety product trademarked as Phycomin® for which no other information is given, nor can be found anywhere on the internet including PubMed, stating that it is concentrated PEA-extract derived from Aphanizomenon flos-aquae. Interestingly enough, however, this patent doesn’t call for using AFA as a source for PEA, but just pure phenylethylamine itself, which anyone can buy at a bulk nutrition shop for next to nothing compared E3Live® BrainON®.
But what about the phenylethylamine added to E3Live®, as the BrainON® component – does it do what the marketing claims? Does it “promote mood balance and enhanced focus”? Unfortunately, an oral dosage of phenylethylamine has at most a very temporary effect in normal individuals. This is due to the presence of a natural enzyme in the body called monamine oxidase (MAO-B), which rapidly breaks down any oral dose of PEA into it’s constituent components. Research pharmacologist Alexander Shulgin states that PEA taken orally in doses up to 1600 mg has no effect, but sensitive individuals may indeed experience a temporary high. Several years ago, researchers thought that phenylethylamine was responsible for the mood altering effects of chocolate, but this was eventually dismissed. To elicit any kind of sustained effect, PEA must be taken with a MAO inhibitor, such as selegiline, deprenyl or Syrian Rue (Peganum harmala), and when this happens, PEA can become a seriously addictive drug. According to the “certificate of analysis” provided above, E3Live® BrainON® contains 1 g of PEA per 100 g of the product, and thus a typical 2-4 gram daily dose of E3Live® BrainON® only contains 200-400 mg of phenylethylamine. Although the PEA in E3Live® BrainON® will have little to no stimulatory effect in healthy individuals, in those taking taking antidepressants or MAO inhibitors, as well as those suffering from schizo-affective disorders in which MAO may be diminished, it could be that a large dose of E3Live® BrainON® could be strong enough to have serious side-effects and/or cause psychosis. Unfortunately, I don’t see this warning stated anywhere on the E3Live® website.
While PEA may have been added to E3Live® BrainON® to boost the claim that it has cognitive benefits, the “rush” that consumers sometimes experience with this product could be something else altogether. As John M. McPartland noted above in his Townsend Letter article, one of the toxins found in Aphanizomenon flos-aquae not apparently tested for in E3Live® BrainON® is anatoxin, which is structurally similar to cocaine and has similar stimulatory effects upon catecholamine secretion as phenylethylamine. Unlike phenylethylamine, however, anatoxin is directly toxic to neurons, and in high doses causes respiratory failure. Unfortunately, the effect of chronic administration of anatoxin isn’t known. Thus while the PEA issue seems to me to be no more than deception, I cannot in good faith recommend to anyone that they ingest neurotoxins to get a “rush”.
The bottom line
Based on the evidence, I can’t recommend to my pregnant patient that she takes this product, and I would council all pregnant women to avoid it as well – even if we just consider the high retinoic acid content. As well, due to its potential neurotoxic effects, I also suggest that children and the elderly avoid this product as well. While I am open to the idea that AFA, like other algae such as Chlorella, might be beneficial for human consumption, I am worried that the levels of hepatotoxins and neurotoxins might be too high in E3Live® products. The only way to resolve this issue is for E3Live® BrainON® to actively publish their testing data and guarantee the safety of this product for regular human consumption.